- Research
- Open access
- Published:
Tethered cord syndrome: surgical outcome of 43 cases and review of literatures
Egyptian Journal of Neurosurgery volume 34, Article number: 4 (2019)
Abstract
Objective
To evaluate the surgical treatment of tethered cord syndrome (TCS), a prospective analysis of 43 patients operated at Neurosurgery Department Zagazig University hospitals from May 2013 to January 2017 with 1 year follow-up had been done.
Patients and methods
Adult and children patients with tethered cord syndrome subjected to microscopic surgeries for release of cord and nerves tethering with exclusion of primary repair of meningiomyelocele, paraplegic patients, hydrocephalic patients, and ages below 2 years old. Magnetic resonance imaging (MRI) of the spine was done for all patients and urodynamic studies for patients more than 6 years old preoperative and postoperative after 1 year of surgery.
Results
Ten patients were adults > 18 years old and male to female ratio was about 2:1. All patients presented with multiple clinical manifestations which either improved or stable during follow-up after surgery. Controllable complications occurred: cerebrospinal fluid (CSF) leak in 18.6% and wound infection in 4.7%. Urodynamic studies improved in 73% of patients after surgery and children showed significant improvement in all symptoms except back pain than adult patients.
Conclusion
Microscopic surgery is of value for patients suffering tethered cord syndrome with low risk of complications.
Introduction
Tethered cord syndrome (TCS) is a stretch-induced functional disorder of the spinal cord with its caudal part anchored by an inelastic structure. The accepted cause of TCS is spinal cord traction, which leads to anatomic and metabolic disorders that are responsible for the clinical presentation. Fixation of the spinal cord can occur congenitally (primary TCS) or in association with other intra-spinal pathologies or postoperative scarring (secondary TCS). Most cases are related to spinal dysraphism [1]. The age at presentation of TCS ranges from early childhood to the 80s. The symptoms related to a congenital tethered cord occur most commonly in childhood, but in many patients, the diagnosis is not established until adulthood. The presentation may also differ according to the underlying pathology, with back and leg pain, cutaneous signs, orthopedic deformities, muscle weakness, urinary dysfunction, and neurological deficits being the most common. Other manifestations include gait deterioration, foot deformities, progressive scoliosis, and sphincter incontinence. Young children may have skeletal growth deformities, such as a leg length discrepancy. Adolescent or young adult patients often complain of unexplained long-term back pain [2].
Decisions about treatment for tethered cord syndrome are complicated. Once the diagnosis established or when there is an established likelihood that tethered cord syndrome is evolving, the neurosurgeon is required to choose among treatment alternatives that will help patients to maintain normal lives while minimizing surgical risks [1].
In this work, we presented a study of 43 patients with tethered cord syndrome to evaluate the clinical presentation, imaging findings of such cases, and results of surgical treatment.
Patients and methods
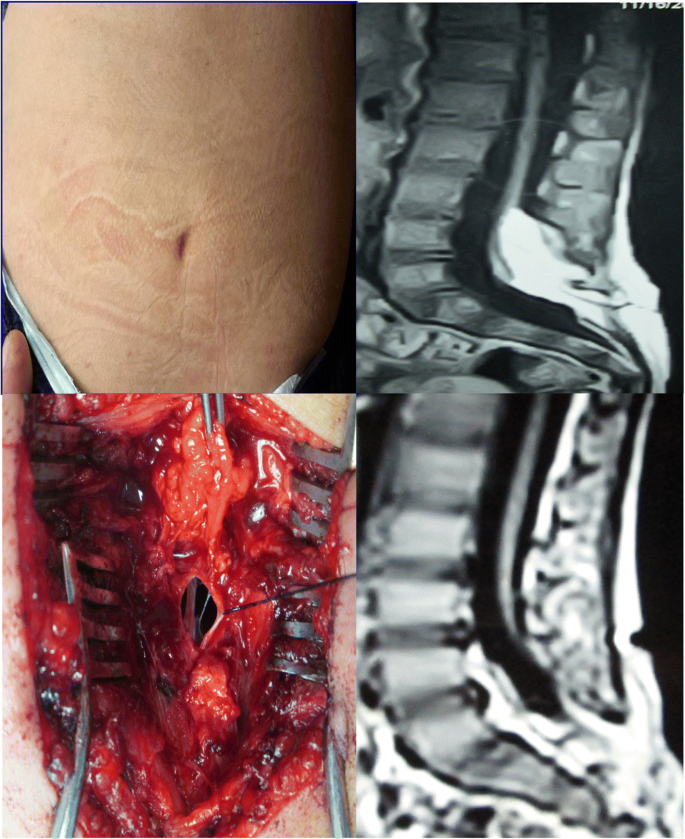
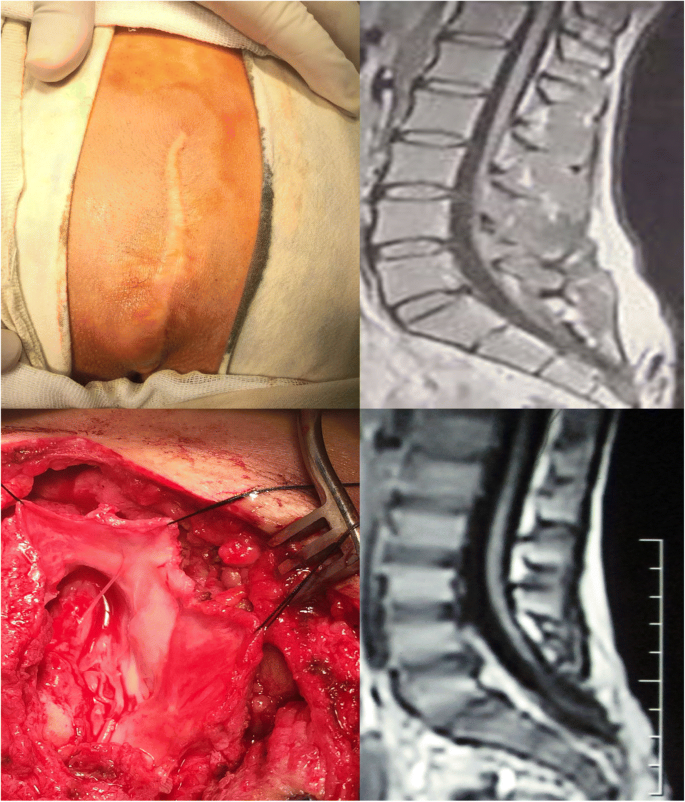
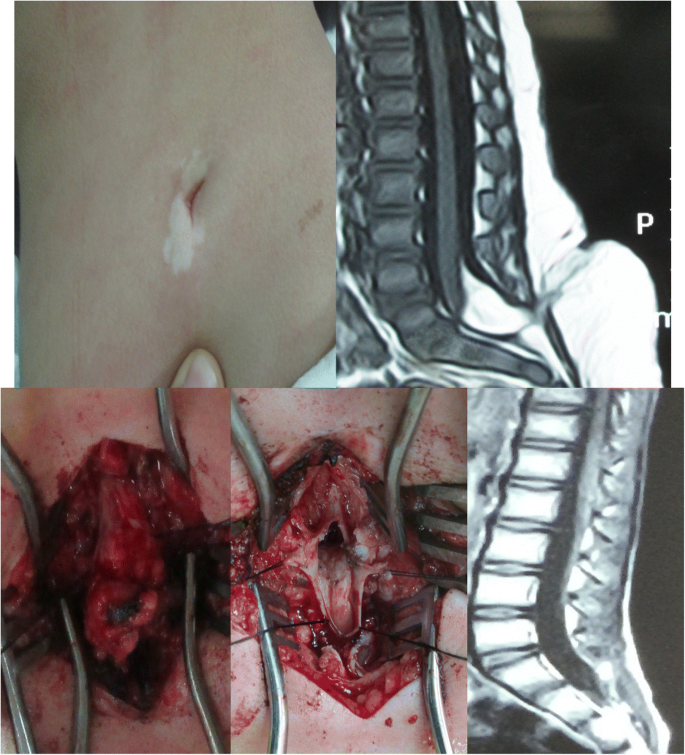
Forty-three patients with tethered cord syndrome, 29 males and 14 females with ages from 2 to 23 years old, were operated at Neurosurgery Department Zagazig University Hospital from May 2013 to January 2017 after approval from the Zagazig University Institutional review board (Zu-IRB). On admission, a written consent was taken for the procedure of untethering under general anesthesia by microscopic surgery. All patients were evaluated for general and neurological condition by clinical, laboratory, and imaging examination. Preoperative MRI of the spine was done for all patients, and urodynamic studies were done for patients more than 6 years old. Clinical evaluation had been done till hospital discharge and then after 3, 6, and 12 months. Urodynamic studies and MRI of the spine repeated after 1 year of surgery. All patients were subjected to microscopic surgeries for untethering under general anesthesia for releasing tethering elements and repair of the thecal sac. Patients included in this study were diagnosed with tethered cord syndrome clinically and by imaging with exclusion of primary repair of meningiomyelocele, paraplegic patients, hydrocephalic patients, and ages below 2 years old. Data collected throughout preoperative and postoperative examination and investigations were analyzed and submitted to statistical procedures using statistical packages for social science (SPSS) version 20. P value was set at < 0.05 for significant results (Figs. 1, 2, 3, 4, and 5).
Results
Patients of this study were 29 males and 14 females with ratio about 2:1, and the youngest was 2 years old and the oldest was 23 years old with a mean age of 9 years (Tables 1 and 2). Table 3 shows the clinical presentation of these patients; back lump was the commonest back sign. Clinical analysis of those patients especially below 6 years old must be taken with consideration of normal physiological and mental development as normal urine control can be considered at age 5 years, stool control at age 4 years, and mental pain/parathesia differentiation at 6 years old. Imaging and urodynamic studies of our patients (Table 4) show spina bifida in 33/43 (77%) patients, lipoma in 20/43 (71%) patients, and conus location at L5 in 35% of the patients. Urodynamic studies show neurogenic bladder abnormalities in all examined patients (15/15, 100%). Microscopic untethering was done for all patients under general anesthesia with operative findings in Table 5 and surgical procedures in Table 6. Intraoperative adhesions were found in 36/43 (84%) patients and released in all patients. Thickened filum terminale was found in 28/43 (65%) patients and sectioned in all patients. Postoperative complications were cerebrospinal fluid (CSF) leak in seven patients, of them two patients needed secondary sutures and two patients suffered wound infection and treated conservatively (Table 7). After 1 year follow-up, there were significant improvements in children compared to adults regarding parathesia, lower limb weakness, urinary abnormalities, and bowel abnormalities (Table 8). Tables 9 and 10 show the significant role of filum sectioning and absence of lipoma in clinical improvement in those patients. Urodynamic study improvements were noted in 11/15 (73%) patients, lipoma size decreased in all affected patients, and conus location changed in only 7% patients at 1 year follow-up (Table 11). Demonstrative cases shown in (Figs. 1, 2, 3, 4, and 5).
Discussion
Most series on tethered cord syndrome showed female predominance [3, 4], while our study showed male predominance (67%).
Tethered cord syndrome is mostly noted in children. There were 23 adult patients versus 50 children with tethered cord treated in Sofuoglu et al. [3] report. In our study, there were 33 children and the 10 adult patients.
Clinical manifestations of TCS differ among patients especially children and adults. The symptoms and signs may be noted since birth or appear later on with body growth as the spines elongate and stretch-induced functional disorders of the spinal cord and roots occur. Clinical manifestations of children in this study were back lump in 70%, skin dimple in 9%, back pain and parathesia from the age of 6 years old in 100% and 67% respectively, lower limb weakness in 61%, urine abnormalities from the of age 5 years in 75%, and bowel abnormalities from the age of 4 years in 65%. The study of Yelikbayev and Tutayeva [5] on 30 children aged 2–18 years reported weakness in 87%, impaired functions of pelvic organs in 90%, and skin manifestations in 77%. Khoshhal et al. [2] study on 35 patients aged 2 months to 11 years found that the most frequent dysraphism was lipomeningomylocele (34.3%) followed by myelomeningocele (22.8%) and dermal sinus (14.3%). Back lump was presented in 65.7%, and neurological impairment in 68.4% of 2 years or older.
Adult patients in this study presented with urine abnormalities in 100%, bowel abnormalities in 80%, back pain in 80%, lower limbs weakness in 60%, and back lump in 50% of the patients. Gao et al. [6] study on 82 adult tethered cord patients found low back pain in 83%, weakness in 71%, sensory dysfunction in 54%, and defecation dysfunction in 50%. Sofuoglu et al. [3] reported clinical manifestations of adult tethered cord as 65.2% back pain, 52.2% bladder dysfunction, 17.4% fecal incontinence, 52.2% weakness, 21.7% numbness, and 61% back swelling.
MRI, plain X-ray of the spine, and urodynamic studies are of great value for diagnosis and management of tethered cord syndrome. We found spina bifida in 33 (77%) patients, lipoma in 20 (47%) patients, dermoid in 3 (7%) patients, conus level at L5 in 15 (35%) patients, and urodynamic studies were impaired in all study cases, mostly hyper-reflexic bladder (67%). Sofuoglu et al. [3] noted in their study on 23 adult patients the commonest conus level was L5 (34.8%), lipoma in 37%, and dermal sinus in 21.7%. Gupta et al. [7] mentioned that the most frequent MRI finding was a low lying spinal cord with intradural and/or extradural lipoma. Yelikbayev and Tutayeva [5] study on children noted hyper-reflexic bladder is often marked, and they considered the tethered cord syndrome as the cause of neurogenic hyper-reflexic bladder even the conus at normal level without filum terminalis changes. In 18–54% of TCS patients, the conus lies at normal level, and diagnosis by dynamic MRI of the spine shows effort-induced symptoms [8, 9], but this not found in our study. Also, conus level varied between studies as Valentini et al. [10] reported L2–L3 level in 50% of patients.
Microscopical treatment was done for all patients dealing of the offending pathologies.
Cerebrospinal fluid leak occurred in eight patients (19%), two of them needed 2ry sutures. Wound infection occurred in two cases and 5% were treated conservatively. Duz et al. [11] reported 5% CSF leak, and no infections in 22 patients. Sofuoglu et al. [3] reported CSF leak in three patients and wound infection in three patients (13%). Rajpal et al. [12] reported 3/61 patients suffered wound infection, one patient suffered CSF leak, two patients suffered pseudomeningocele, and one patient suffered acute respiratory distress syndrome. Iskandar et al [13] reported one CSF leak and five pseudomeningocele in their study on 34 patients.
Clinical improvement 1 year after surgery in our study showed back pain improvement in 60% of children and 75% of adults, parathesia improved in 60% of children and 30% of adults, weakness improved in 40% of children and 17% of adults, urine abnormalities improved in 60% of children and 30% of adults, and bowel abnormalities improved in 47% of children and 25% of adult patients. Children in our study showed significant improvement regarding all symptoms except back pain in comparison with adults. Intraoperative filum sectioning showed significant improvement of patient symptoms except back pain, and absence of lipoma showed significant improvement in weakness. Review of literatures suggests that the tethered cord syndrome reversible symptoms are due to metabolic derangement and alterations in oxidative metabolism. Persistent symptoms may vary depending on severity and duration at presentation [8]. Iskandar et al. [13] found improvement in adults, 81.5% back pain, 43.1% motor or sensory dysfunctions, and 61.1% bowel and bladder disturbance. Sofuoglu et al. [3] reported 50% improvement in back pain, 66.7% motor weakness improvement, and 75% bladder and bowel improvement in adults. Lee et al. [1] found improvements in 78% back pain, 83% leg pain, 64% motor weakness, and 50% urological abnormalities. Duz et al. [11] reported back pain improvement in 57.1% and bladder dysfunction in 66.6%, and two patients with fecal incontinence did not improve. Rajpal et al. [12] reported back pain improved in 65% and bowel/bladder dysfunctions in 62%. Solmaz et al. [14] reported urological improvement in 21 patients (20%) and back pain improved in all patients on their study on 49 children. In Bowman et al. [15] study on children with myelomeningocele for untethering, the pain improved in 100%, and 70% showed improvement in lower extremities and 64% in bladder dysfunctions. Haro et al. [16] reported that adults showed better improvement in neurological and urinary problems than natal or juvenile onset tethered cord syndrome. Seki et al. [17] mentioned that age at surgery is not significantly associated with prognosis. Tethered cord syndrome may have different curative effect after surgery according to the cause. Removal of the thickened filum can get better results [6]. Recurrent surgeries and presence of lipoma had higher incidence of failed detethering [10]. Also, Selden et al. [18] found significant improvement with filum sectioning. These data agree with our results.
Conus location detected by MRI on follow-up found to be on the same location as preoperative MRI in 77% of the patients in our study, and urodynamic studies showed improvement in 73% of the studied patients. Postoperative MRI has no role for evaluation of good detethering but only clinical and urodynamic evaluation. Even the presence of lipoma residual is not significantly associated with retethering [19]. Kearns et al. [20] found 44% improvement in urodynamic studies on 34 children after tethered cord repair and mentioned that a review of five series showed improvement in 11.1–54.5% after untethering, but none of their patients or other studies became urologically normal as the conus and roots were inevitably exposed to some injuries, also documented by [21, 22]. Improvement of urological symptoms or urodynamic finding reported to be 38% and 100% respectively by Vernet et al. [23] and Flanigan et al. [24].
Conclusion
Clinical presentation of tethered cord syndrome differs according to underlying pathology and age of the patients. There were improvements in patient conditions in all studies with few controllable complications. Surgical treatment is beneficial in most patients, and childhood intervention is better than adulthood. Postoperative MRI findings not necessarily correlate with surgical outcome but clinical and urodynamic studies are the best predictors.
Study limitations
-
1.
The causes of tethered cord syndrome are so much and in need for a bigger number of cases for evaluation.
-
2.
The follow-up evaluation was 1 year only, which is a short period.
Abbreviations
- CSF:
-
Cerebrospinal fluid
- MRI:
-
Magnetic resonance imaging
- TCS:
-
Tethered cord syndrome
References
Lee GY, Paradiso G, Totor CH, Gentili F, Massicotte EM, Fehlings MG. Surgical management of tethered cord syndrome in adults: indications, techniques, and long-term outcome in 60 patients. J Neurosurg Spine. 2006;4(2):123–31.
Khoshhal KI, ABOS MWR, Elgamal EA, Salih MAM. Tethered cord syndrome: a study of 35 patients. J Taibah University Med Sci. 2012;7(1):23–8.
Sofuoglu OE, Abdullah A, Emel E, Guler B. Management of tethered cord syndrome in adults: experience of 23 cases. Turk Neurosurg. 2017;27(2):226–36.
Klekamp J. Tethered cord syndrome in adults. J Neurosurg Spine. 2011;15:258–70.
Yelikbayev GM, Tutayeva AA. Clinical manifestation of a tethered cord syndrome at children, and research methods for early diagnosis of disease. Biomed Pharmacol J. 2015;8(2):597–601.
Gao J, Kong X, Li Z, Wang T, Li Y. Surgical treatment on adult tethered cord syndrome. A retrospective study. Medicine. 2017;96(32):e7808.
Gupta SK, Khosla VK, Sharma BS, Mathuriya SN, Pathak A, Tewari MK. Tethered cord syndrome in adults. Surg Neurol. 1999;52(4):362–70.
Yamada S, Won DJ, Siddiqi J, Yamada SM. Tethered cord syndrome: overview of diagnosis, and treatment. Neurol Res. 2004;26:719–21.
Warder DE, Oakes WJ. Tethered cord syndrome: the low lying, and normally positioned conus. Neurosurg. 1994;34:597–600.
Valentini LG, Selvaggio G, Visintini S, Erbetta A, Scaioli V, Solero CL. Tethered cord: natural history, surgical outcome, and risk for Chiari malformation 1 (CM1). Neurol Sci. 2011;32(3):353–6.
Duz B, Gocmen S, Secer HI, Basal S, Gonul E. Tethered cord syndrome in adulthood. J Spinal Cord Med. 2008;31(3):272–8.
Rajpal S, Tubbs RS, George T, Oakes WJ, Fuchs HE, Hadley MN, Iskander BJ. Tethered cord due to spina bifida occulta presenting in adulthood: a tricenter review of 61 patients. J Neurosurg Spine. 2007;6(3):210–5.
Iskandar BJ, Flumer BB, Hadley MN, Oakes WJ. Congenital tethered spinal cord syndrome in adults. Neurosurg Focus. 2001;10(1):e71–5.
Solmaz I, Izci Y, Albayrak B, Cetinalp E, Kural C, Sengul G, Gocmez C, Pausal S, Tuzun Y. Tethered cord syndrome in childhood: special emphasis on the surgical technique, and review of the literature with our experience. Turk Neurosurg. 2011;21(4):516–21.
Bowman RM, Mohan A, Itot J, Mclone DJ. Tethered cord release: a long-term study in114 patients: clinical article. J Neurosurg Pediatr. 2009;3(3):181–7.
Haro H, Komori H, Okawa A, Kawabata S, Shinomiya K. Long-term outcome of surgical treatment for tethered cord syndrome. J Spinal Disord Tech. 2004;17(1):16–20.
Seki T, Hida K, Yano S, Sasamori T, Hamauch S, Koyanagi I, Houkin K. Surgical outcome of children, and adolescents with tethered cord syndrome. Asian Spine J. 2016;10(5):940–4.
Selden NR, Nixon RR, Skoog SR, Lashley DB. Minimal tethered cord syndrome associated with thickening of the terminal filum. J Neurosurg. 2006;105(3):214–8.
Schoenmakers MA, Gooskens RH, Gulmans VA, Hanlo PW, Vandertop WP, Uiterwaal CS, Helders PJ. Long-term outcome of neurosurgical untethering on neurosegmental motor and ambulation levels. Dev Med Child Neurol. 2003;45:551–5.
Kearns JT, Esposito D, Dooley B, Frim D, Guandeti MS. Urodynamic studies in spinal cord tethering. Childs Nerv Syst. 2013;29:1589–600.
Gross AJ, Michael T, Godeman F, Weigel K, Huland H. Urological finding in patients with neurosurgically treated tethered spinal cord. J Urol. 1993;149:1510–1.
Paradiso G, Lee GY, Sarjeant R, Fehlings MG. Multi-modality neurophysiological monitoring during surgery for adult tethered cord syndrome. J Clin Neurosci. 2005;12(93):935–7.
Vernet O, Farmer JP, Houle AM, Montes JL. Impact of urodynamic studies on the surgical management of the spinal cord tethering. J Neurosurg. 1996;85:555–9.
Flanigan RC, Russel DP, Walsh JW. Urologic aspect of tethered cord. Urology. 1989;33:80–3.
Acknowledgements
Not applicable.
Funding
No funding was received for this study.
Availability of data and materials
All data that support the findings of this study are available from the neurosurgery department Zagazig university hospital. Data are however available from the authors when requested with permission.
Author information
Authors and Affiliations
Contributions
WAAE, AKAA, and SHM contributed to the study conception, design, and surgical works. WAAE collected data and drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
A written consents were obtained for all patients ( from the patient and from the parent when age below 16 years old ), and the study approved by Zagazig university institutional review board (Zu-IRB) on 15/3/ 2013.
Consent for publication
A written consents for publication from the patients and from parents when the age below 16 years old were attained.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Elmesallamy, W., AbdAlwanis, A. & Mohamed, S. Tethered cord syndrome: surgical outcome of 43 cases and review of literatures. Egypt J Neurosurg 34, 4 (2019). https://doi.org/10.1186/s41984-019-0029-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41984-019-0029-8